Biliary
THE QUESTION: HAVE THESE SYMPTOMS A BILIARY CAUSE?
Abdominal pain is one of the most frequent complaints in the ED, representing 5 to 10% of total consults. In particular, cholelithiasis is responsible for a range of emergency presentations, and its prevalence is 10 to 20% in western countries. In Chile, the prevalence reaches 50% in middle age women, being asymptomatic in 45% of cases. Ultrasound (US) is a quick and harmless bedside tool for detecting biliary disease among patients presenting with abdominal pain, and can answer several specific questions:
Is there cholelithiasis? This is probably the fundamental question and the only one that can be confidently and accurately answered by an emergency physician.
Is there cholecystitis? Acute cholecystitis is often caused by the impaction of gallstones in the Gallbladder (GB) neck or cystic duct. Diagnosis requires a combination of clinical features, sonographic Murphy’s sign, impacted gallstone, GB wall thickening > 3 mm, and/or pericholecystic fluid.
Is there choledocholithiasis? Usually, a combination of luck and expertise is required to image this. Its presence may be inferred by a dilated common bile duct, but recall there are many other causes of CBD dilation.
Is the common bile duct dilated? This is a crucial question in the patient with a picture of cholangitis or jaundice. Although it can be challenging to demonstrate an obstructing stone, it is possible to image the CBD and measure its size.
Rationale.
WHY USE ULTRASOUND?
US is capable of accurately assessing the presence of gallstones and the size of the bile duct, while at the same time can provide differential diagnosis, making it the initial test of choice for suspected biliary disease. Furthermore, it is usually readily available and practical in the ED, as moving patients to the radiology bay is time-consuming and may not always be feasible or safe, especially in unstable patients or those actively vomiting.
In the ED, specifically for the diagnosis of cholelithiasis, the POCUS learning curve is relatively short, and the accuracy has a good correlation with the specialist, as sensitivity is reported between 86% to 96% with a specificity up to 88%. This variability is due to the operator-dependent nature of sonography [4,5].
LIMITATIONS
While emergency US can accurately diagnose cholelithiasis, the same cannot be said for the diagnosis of cholecystitis, as both sensitivity and specificity for sonographic signs of acute cholecystitis are significantly lower. Moreover, the learning curve to reliably determine findings such as CBD dilation, GB wall thickening, or pericholecystic fluid is not only longer but also more complex, and likely to require ongoing feedback and teaching along the way [4]. As a result, an additional imaging technique (radiologist-performed US) may be necessary to rule out or confirm the diagnosis of cholecystitis confidently.
Given the high sensitivity of US for cholelithiasis, the absence of gallstones has been proposed as a validated method for ruling out acute calculous cholecystitis in the ED [6]. It should be considered, however, the possibility of acute acalculous cholecystitis, as it represents a life-threatening condition accounting for up to 14% of all cholecystitis cases. Admittedly, though, it classically occurs in already hospitalised critically ill patients with specific risk factors, and who conform a different population than those presenting to the ED with abdominal pain [7].
PITFALLS
As the bile ducts are tubular structures adjacent to blood vessels, there may be a resemblance between both. Hence, experience and doppler are required to confidently identify the bile ducts, particularly when they are intrahepatic [1]. Additionally, small stones (<5 mm diameter) will lack the classic acoustic shadows of larger stones, potentially leading to false negatives. Conversely, the air in the duodenum adjacent to the GB may cast a “dirty” shadow which could translate into a false positive.
By this point, it should be clear that emergency US does not replace formal upper abdominal US, as the latter is complex and includes the assessment of the liver parenchyma, intrahepatic bile ducts, pancreas and other structures. Such investigations are not part of the focused RUQ POCUS. In the ED, stick to the gallbladder and common bile duct.
The gallbladder rests nestled between two lobes (right and quadrate) on the inferior aspect of the liver, and it can be divided into neck, body and fundus. The gallbladder’s exact location and shape are highly variable, depending on volume, oral intake and anatomical divergence. Size is also variable, yet < 4 cm in diameter and < 10 cm in length are usually accepted as normal. A larger gallbladder defines distension and might be suggestive of an impacting stone. A wall thicker than 3 mm is also abnormal.
The apex of the gall bladder is called the fundus, which then becomes the main body before narrowing to the neck and eventually the cystic duct. The position of the gallbladder’s neck is the least variable and can be found close to the portal vein via the major lobar fissure.
Anatomy.
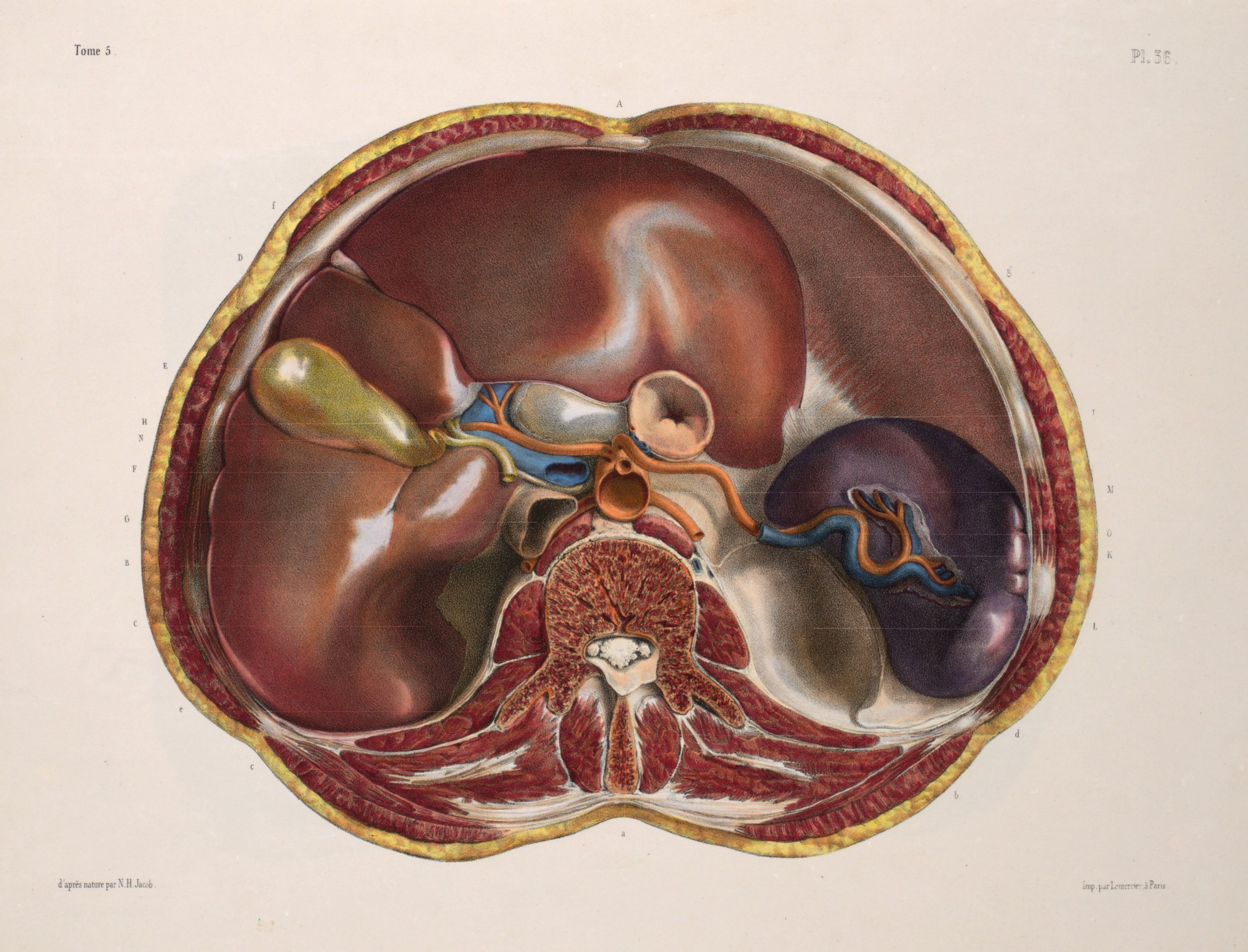
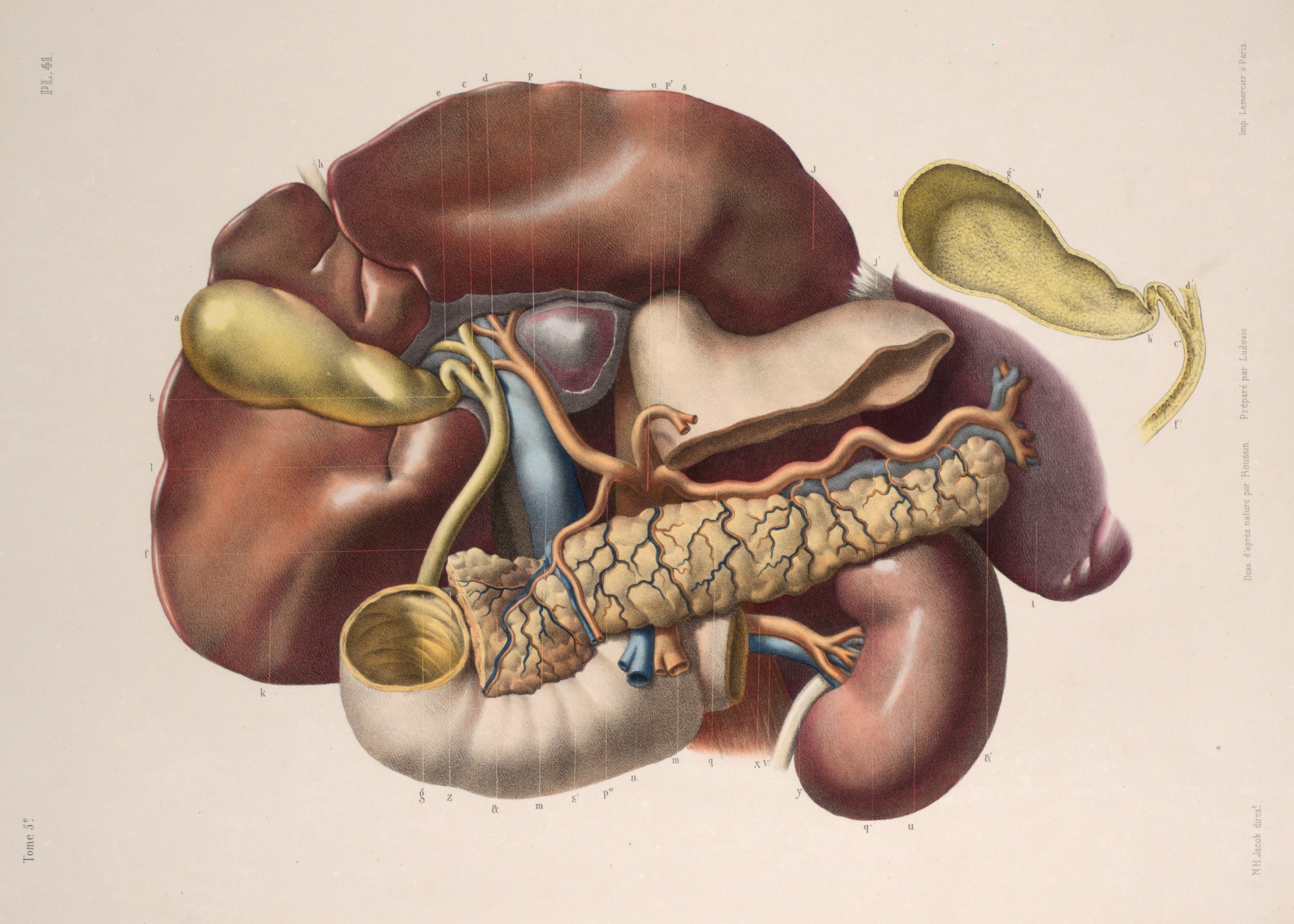
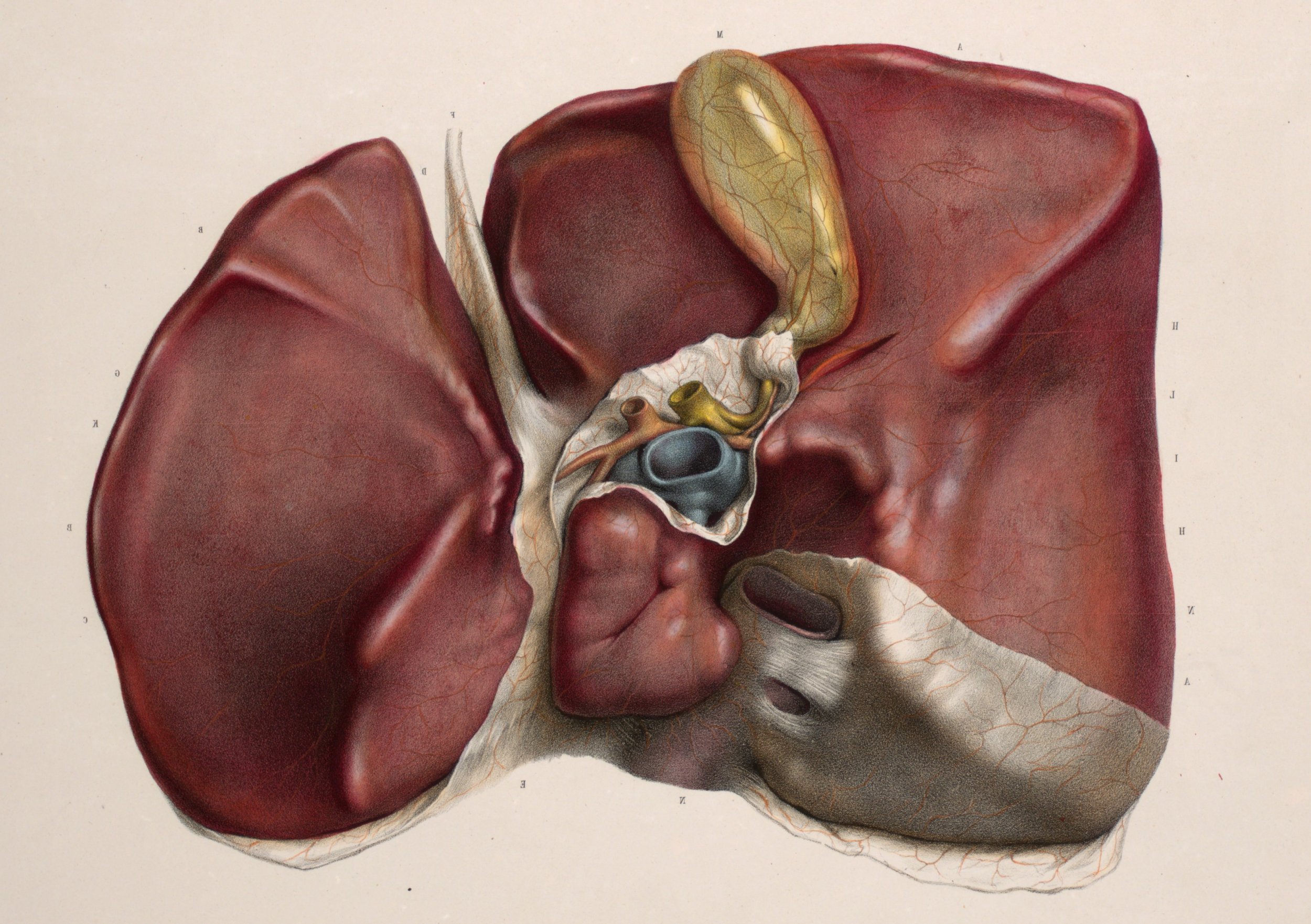
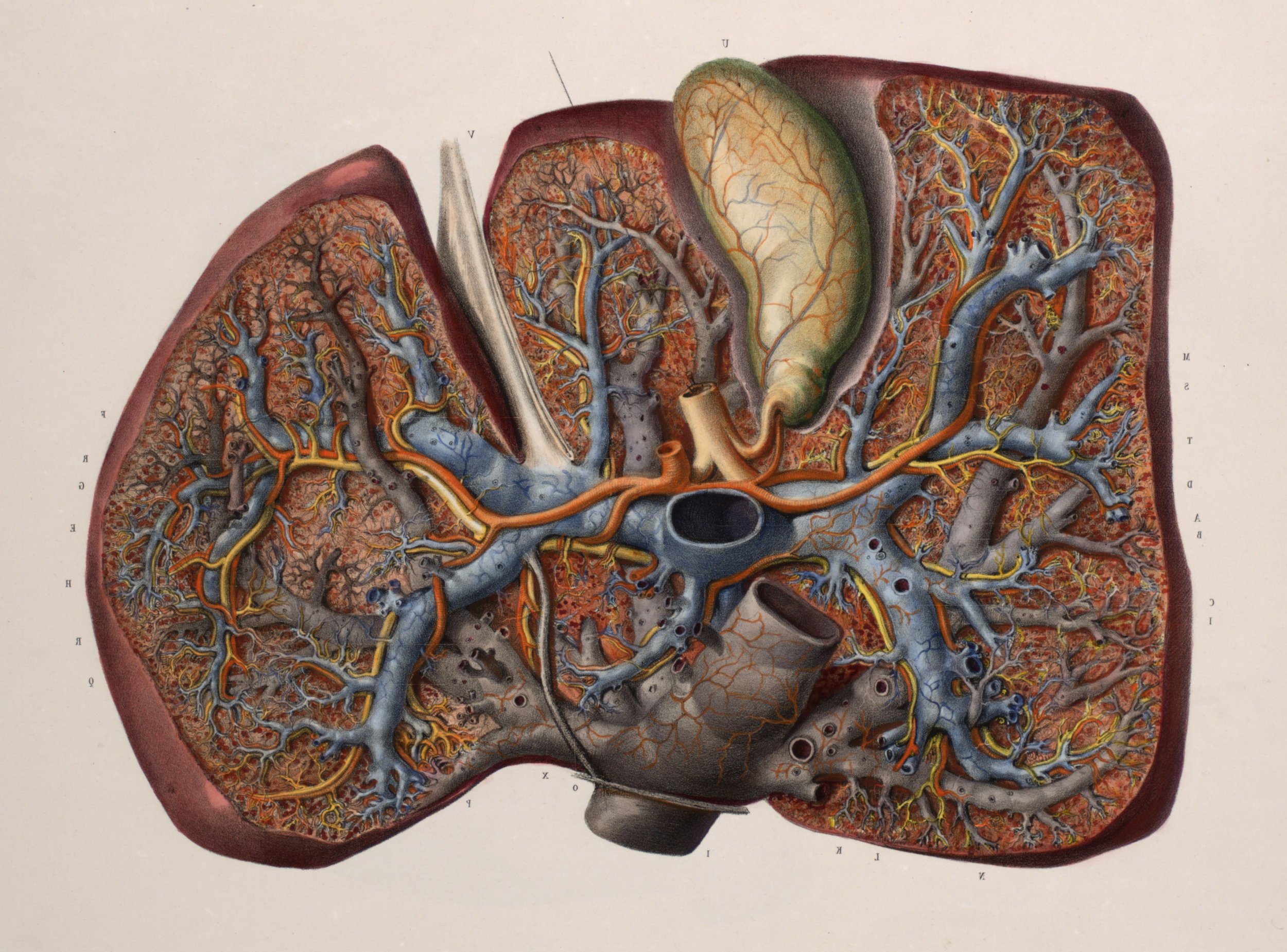

The normal cystic duct is 2-3 cm in length and < 2 mm diameter. The cystic duct meets with the common hepatic duct to create the common bile duct (CBD – choledocus), which then descends in the hepatoduodenal ligament anterior to the portal vein and with the hepatic artery on its left. Lastly, it joins the pancreatic duct at the ampulla of Vater and empties into the duodenum. The normal CBD diameter is 6 mm or less.
Technique & Views.
PROBE
The curved low-frequency probe is of choice as it provides enough depth to visualise deeper structures. It should be used in the standard abdominal setting.
PATIENT’S POSITION
The supine position is the most practical, and both deep inspiration and raising the patient’s right arm will improve visualization. If it is still difficult to obtain a proper image, positioning the patient in a left lateral decubitus, displacing the duodenum, is likely to facilitate the views.
Consider that the gallbladder empties its content after meals and therefore is harder to view if the patient has recently eaten. Also, the walls may appear thicker because of physiological GB contraction. More than one window, scanning plane and patient position are required to view the GB adequately.
THE VIEWS
Place the probe under the xiphoid process with the marker to the patient's head, and slide it across the costal margin towards the mid-axillary line. The fasted gallbladder appears as a well-demarcated, fluid-filled structure located at the medial-inferior edge of the liver. The gallbladder narrows down towards the neck, where the portal vein lies. Confirm that you are actually scanning the GB by identifying the portal triad and the “exclamation sign”.
LONGITUDINAL VIEW
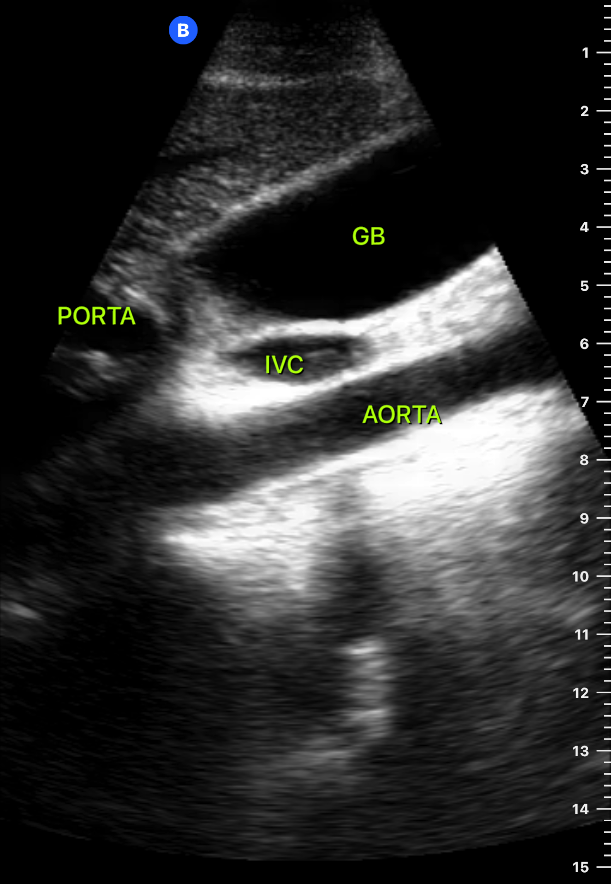
Align the probe with the GB long axis to reveal the longitudinal view and scan through it while altering the probe angle to assess the fundus, body and neck properly. Depending on the patient’s habitus and anatomy, you will also visualise the IVC and Abdominal Aorta. Take a second to identify the structures accurately.
TRANSVERSE VIEW
A 90º degree rotation to the right will show the gallbladder in transverse view. Fan the probe to assess from fundus to neck, and be sure to scan as much of the GB as possible to avoid missing localized pathology. Be aware that a content-filled duodenum can resemble a large stone occupying the gallbladder; hence, it is essential to be able to differentiate between both.
Cholelithiasis.
Classically, GB calculi are described as intraluminal hyperechoic images that cast posterior acoustic shadows. If not impacted, they should also be mobile and have gravitational dependence. Consequently, scanning the patient in more than one position may elucidate an impacted gallstone, as it will not move with gravity. Neither a very small stone (<5 mm diameter) nor sludge will cast a posterior shadow, although multiple small calculi (microlithiasis) may present poorly defined shadowing.
WALL ECHO SHADOW
If the gallbladder is completely filled with stones, the normal fluid-filled structure with posterior enhancement is no longer seen. Instead, the wall echo shadow (WES) sign can be found as two parallel bright lines with a large posterior shadowing. The bright line closest to the probe is the GB wall and the line beneath represents the echogenic calculi. WES is important because it may be misinterpreted as a bowel loop, when in fact represents cholelithiasis.
Be mindful that not every echogenic image inside the GB lumen is a stone. Neither gallbladder polyps nor sludge will cast acoustic shadowing, the latter, however, has gravitational dependence, while polyps do not move when repositioning the patient.
Cholecystitis.
The diagnosis of acute cholecystitis involves clinical features, inflammatory markers, and characteristic image findings. The classic ultrasound findings are wall thickening > 3 mm, sonographic Murphy’s sign, pericholecystic fluid, and/or impacted gallstone with a distended GB. Yet, as discussed earlier, accurate identification of these signs can be difficult and involves a complex learning curve. Particularly for the novice, confidently ruling out cholecystitis by ultrasound is likely to require the experience of a radiologist.
The normal adult wall thickness is 3mm or less, but normal GB walls will also be thickened due to contraction, which is important to remember in the non-fasted ED population. The GB wall should be measured perpendicular to the long axis and at the anterior wall only, as the liquid inside the GB generates enough acoustic enhancement to make the posterior wall appear falsely thickened. A thickened wall may be seen as two echogenic lines with a hypoechoic region between them (double line sign). Wall thickening suggests acute inflammation and oedema, but can be found in other disease states such as congestive heart failure, sepsis, ascites, renal failure, HIV or and multiple myeloma.
The sonographic Murphy’s sign is assessed by applying pressure with the transducer over the GB. If this reproduces the patient’s pain, it is considered positive and strongly suggest acute GB disease. Pericholecystic free fluid can be found in acute cholecystitis and speaks of a more advanced inflammation stage. However, it may also be found in other disease states, namely pancreatitis, cirrhosis and ascites. An impacted gallstone will not move if the patient is repositioned, and will usually be accompanied by GB distension. Remember that proper interpretation of the images can only be achieved if the GB is visualised in its entire length, including fundus, body and neck. When the image is incomplete (WES) or non-definitive, a formal study or another imaging modality is needed.
Common Bile Duct.
The CBD runs besides and anterior to the portal vein, therefore this is usually the best place to measure it. Identify the GB neck which narrows down towards the portal triad. The large portal vein lies anterior to the inferior vena cava (IVC) and is usually easy to identify. The CBD lies along the front of the vein and has a substantially smaller calibre with very echogenic walls, while the right hepatic artery crosses between the two. The use of colour doppler aids to distinguish the vessels from the CBD. Asking the patient to hold his/her breath in full inspiration will bring the structures into better view and allow the use of Doppler without movement artefact.
The diameter of the CBD is measured from inner to inner wall at the point where is widest. A CBD diameter greater than 6 mm suggests CBD dilation. However, a diameter between 6 to 8 mm needs clinical correlation and can be considered normal in post-cholecystectomy patients. A CBD diameter > 10 mm is always abnormal.
Nonetheless, the measurement of the CBD may not be essential for all patients. Recent evidence suggests that in patients with normal laboratory values and without other sonographic findings of GB pathology, the suspicion for isolated choledocholithiasis is not justified and CBD measurement is unlikely to contribute to the evaluation of these patients. (8) Needless to say, in patients with a clinical picture of jaundice or suspected cholangitis, CBD measurement can provide valuable and determining information.
Author: Felipe Urriola Perez | Published: 31 October 2022
Reference.
Bowra, Justin; McLaughlin, Russell; Atkinson, Paul; Henry, Jaimie. Emergency Ultrasound Made Easy, Third Edition. 2022. Elsevier Health Sciences.
Basaure, Carlos; Clausdorff, Hans; Riquelme; Felipe. Ultrasonido Clínico, First edition. 2018. Emergency Medicine Residency Program, Universidad Católica de Chile.
The Pocus Atlas. https://www.thepocusatlas.com/hepatobiliary-1
Jang, T. B., Ruggeri, W., Dyne, P., & Kaji, A. H. (2010). The Learning Curve of Resident Physicians Using Emergency Ultrasonography for Cholelithiasis and Cholecystitis. Academic Emergency Medicine, 17(11), 1247–1252. PMID: 21175524
Ross M, Brown M, McLaughlin K, Atkinson P, Thompson J, Powelson S, Clark S, Lang E. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011 Mar;18(3):227-35. PMID: 21401784
Villar J, Summers SM, Menchine MD, Fox JC, Wang R. The Absence of Gallstones on Point-of-Care Ultrasound Rules Out Acute Cholecystitis. J Emerg Med. 2015 Oct;49(4):475-80. PMID: 26162764
Indar AA, Beckingham IJ. Acute cholecystitis. BMJ. 2002 Sep 21;325(7365):639-43. PMCID: PMC1124163
Lahham S, Becker BA, Gari A, Bunch S, Alvarado M, Anderson CL, Viquez E, Spann SC, Fox JC. Utility of common bile duct measurement in ED point of care ultrasound: A prospective study. Am J Emerg Med. 2018 Jun;36(6):962-966. PMID: 29162442